- Human metapneumovirus (HMPV) is a virus that can cause lung and breathing problems in people of all ages. But it’s especially risky for babies, older adults and people whose immune systems aren’t normal. First discovered in 2001, this was a virus. Since then medical doctors, scientists and health care authorities have been researching the how it spreads, how it affects the body and what can be done to treat it.
- Since this article pulls together everything you need to know about HMPV, it is easier for people, doctors and researchers to learn about HMPV. The aim is to increase awareness and understanding to such an extent that we can be better protected, and help protect others, from its reach.
1. HMPV, and why should you care?
HMPV is a virus that causes respiratory infection. Though not as famous as flu or COVID-19, it is silently giving people illnesses particularly during winters.
- Researchers in the Netherlands found it in 2001. But scientists think it’s been around for decades.
- The disease can affect people of all ages, but kids below 5 years, elderly people and those with weak immunity are most susceptible.
- Why do Indians need to know about it?
- In a family oriented country like India (where we live in congested small apartments with small balconies, travel in crowded trains and crowded buses, suffer from pollution), understanding these viruses is very important. This can help us to prepare and prevent going to the hospital, needlessly.
For further details about respiratory viruses, see WHO’s guide on respiratory health.
2. How Does HMPV Spread?

Just like the flu or common cold, HMPV spreads through:
- Tiny droplets containing the virus are dropped into the air when someone infected coughs and sneezes
- Public places – You might catch the virus if you touch surfaces – like a door handle or phone – that have been contaminated, and then touch your nose or mouth.
- Hugs, handshakes, breathing close together with someone infected, or touching an infected person’s eyes, nose or mouth can all spread it.
3. Symptoms: How to Identify HMPV?
HMPV symptoms are similar to a cold or flu, but range from mild to severe.
Mild Symptoms:
- Runny nose
- Cough
- Sore throat
- Low fever
- Fatigue
Severe Symptoms (especially in kids and elderly):
- A whistling sound if you breathe in (wheezing)
- Breathing difficulty
- High fever
- Chest congestion
- Or in extreme cases, pneumonia or bronchiolitis.
💡 Pro Tip for Parents: Call your doctor if your child’s cough goes on more than a week or if you think your child is having trouble breathing. Healthline provides you with the trusted advice about child health.
4. Who is Most at Risk?

While anyone can get HMPV, certain groups are more vulnerable:
- Babies and toddlers: They have not finished developing their immune systems.
- Elderly people: Aging weakens immunity.
- People with weak immunity: Individuals with cancer patients, organ transplant recipients, or HIV/AIDS.
- Chronic illness patients: People with asthma, diabetes or heart related diseases.
5. Diagnosing HMPV: What Do Doctors Do?
If your symptoms are serious or prolonged, your doctors may suggest testing. Common tests include:
- RT-PCR Test: It’s like a COVID 19 test, just more precise.
- Antigen Tests: Quick but less reliable.
- Chest X-rays: To look for pneumonia or other lung problems.
Do you need reliable diagnostic services? Head over to one of Dr. Lal Path Labs, one of India’s trusted pathology labs.
6. Treatment: How to Manage HMPV at Home?

Unfortunately, there’s no particular medicine yet for HMPV. The symptoms are mostly treated by doctors. Here’s what you can do:
At-Home Care:
- Stay Hydrated: Drink warm water, soups, or herbal teas and keep drinking.
- Steam Inhalation: Helps clear nasal congestion.
- Rest: Don’t go back to work or school too quickly. Give your body time to heal.
- Use Paracetamol: Body aches and fever (consult your doctor for dosage).
When to Go to the Hospital?
- If you, or your child can’t breathe.
- More than 3 days of high fever.
- Severe chest pain or wheezing.
For more information about managing respiratory illnesses visit Mayo Clinic’s Respiratory Health Guide.
7. How to Prevent HMPV?
In India, prevention is always better than cure, and especially in cases where you do not have access to healthcare.
Simple Prevention Tips for Indian Households:
- Wash Hands Often: You need to use soap and water for at least 20 seconds.
- Avoid Crowded Places: Especially during flu season.
- Disinfect Surfaces: Clean your phone, your door handles, your kitchen counters regularly.
- Wear a Mask: If you have symptoms, or you’re visiting crowded places.
For more details on hygiene practices, consult CDC’s Hygiene Tips.
8. How is HMPV Different from Flu and RSV?
| Feature | HMPV | Flu (Influenza) | RSV (Respiratory Syncytial Virus) |
|---|---|---|---|
| Discovery Year | 2001 | 1930s | 1956 |
| Vaccine Available | No | Yes | No |
| Symptoms | Mild to severe respiratory | Fever, body ache, fatigue | Wheezing, severe in infants |
| Peak Season | Late winter to spring | Winter | Fall to early spring |
8.1 . Comparison with Other Respiratory Viruses
| Virus | HMPV | RSV | Influenza |
|---|---|---|---|
| Discovery Year | 2001 | 1956 | 1930s |
| Population Affected | All ages; severe in infants/elderly | Mainly infants and young children | All ages |
| Vaccine Available | No | No | Yes |
9. Current Research on HMPV
We already handle viruses — our scientists are working even harder to know more about HMPV. Globally, researchers are:
- Immunity after infection with HMPV.
- Working on vaccine against the virus’s F protein.
- Looking at the possibility of antiviral drugs which could treat severe cases.
Find out about the latest breakthroughs here with Nature Research.
10. Prevention of HMPV
Because specific treatments or vaccines do not exist, good health practices are of the most importance.
Hygiene Practices:
- Frequent handwashing.
- Not touching the face mainly the eyes, nose and mouth.
Protecting Vulnerable Populations:
- Where masks are required in the crowded or healthcare setting.
- Ensures for isolation of infected individuals so they will not spread.
Research on Vaccines:
- Recent preclinical and early clinical trials suggest that several candidate vaccines based on the F protein exist.
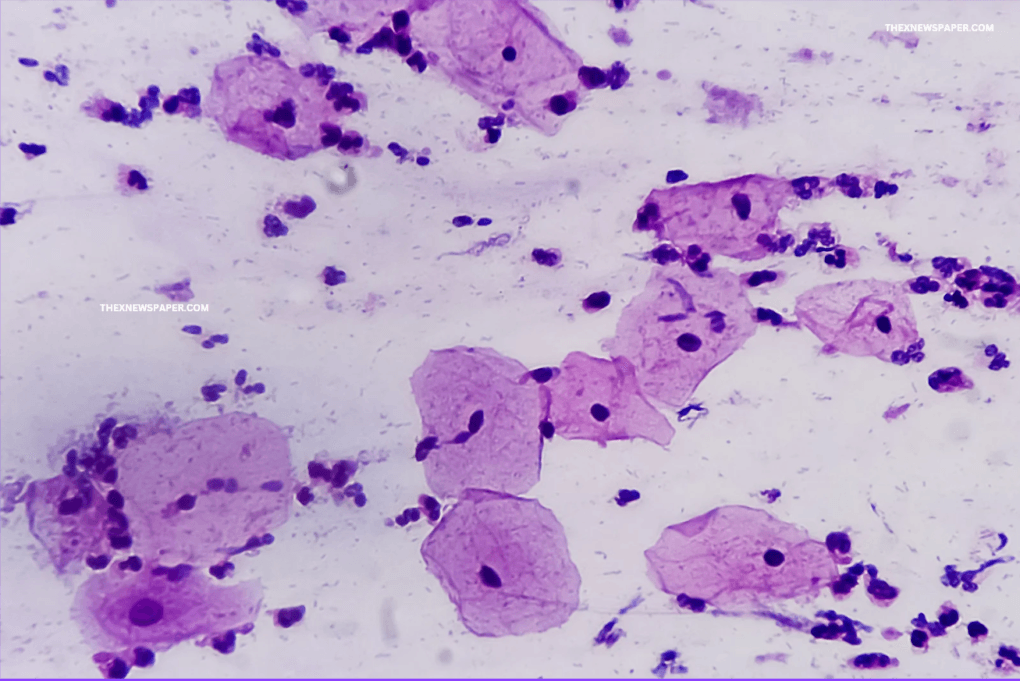
11. HMPV Structure and Virology
Knowledge of HMPV structure is important to vaccine and antiviral therapy developers.
- Genomic Structure: HMPV is an enveloped negative sense single stranded RNA virus. Its genome encodes several structural and non-structural
proteins:
- F Protein: It is key target for vaccine development because it is responsible for viral fusion with host cells.
- G Protein: Can attach to host cells for the attachment of a viral.
- SH Protein: Scientists don’t know exactly what it does but do think it could help the virus escape immune responses.
- Genotypes: HMPV is further classified into two main groups, A and B, with subgroups A1, A2, B1, B2. The genotypes described here circulate globally in co-circulation with other respiratory viruses.
12. FAQs
Q1. How bad could long term problems with HMPV be?
For most people, it’s a short term illness. For kids or elderly patients, however, it can result in pneumonia or asthma flare ups.
Q2. Is HMPV seasonal in India?
Like flu season, it does peak in the winter and early spring.
Q3. Does HMPV spread in schools?
Kids play — and play with each other — so yes, schools can be hotspots for HMPV outbreaks.
Q4: Does HMPV re-infect a person?
Reinfections are common, but immunity to HMPV isn’t lifelong and may have milder symptoms.
Q5: Is HMPV a pandemic risk?
Though easily transmitted, HMPV has a slower mutation rate than influenza or coronaviruses so it’s very unlikely to spread to that level.
Q6: What is the difference between RSV and HMPV?
Both HMPV and RSV are related by symptoms and patients risk, but are different viruses with dissimilar genetic and antigenic properties.
